Prevention of Urinary Tract Infection (UTI) in Neurogenic Bladder (NGB)
Mediverse Blog
Catagories:
Academic articles,
Med News,
Mediverese special
Urinary Tract Infection Prevention in Neurogenic Bladder-
Introduction:
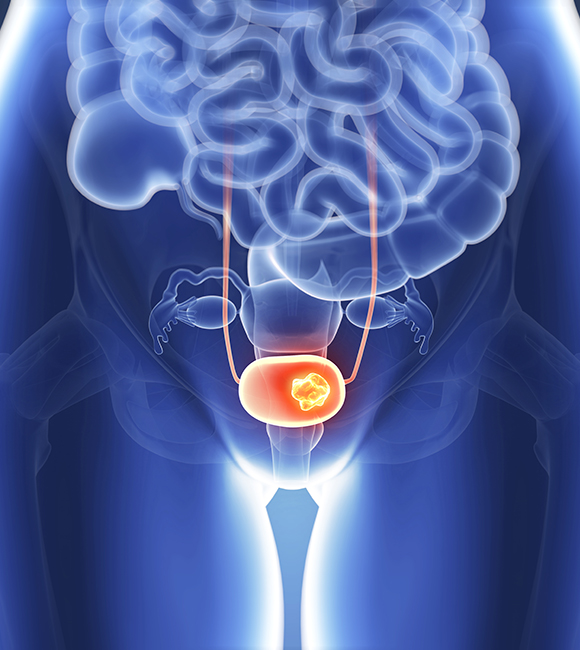
Patients with neurogenic bladder (NGB), caused by central or peripheral nervous system disorders such as spinal cord injury (SCI), multiple sclerosis (MS), spina bifida (SB), cerebral palsy, or Parkinson’s disease, often experience impaired bladder function. Urinary tract infections (UTIs) are the most common complication in this population, with an average rate of 2.5 episodes per patient per year, posing a significant burden on healthcare systems.
Management:
1. Catheter Management:
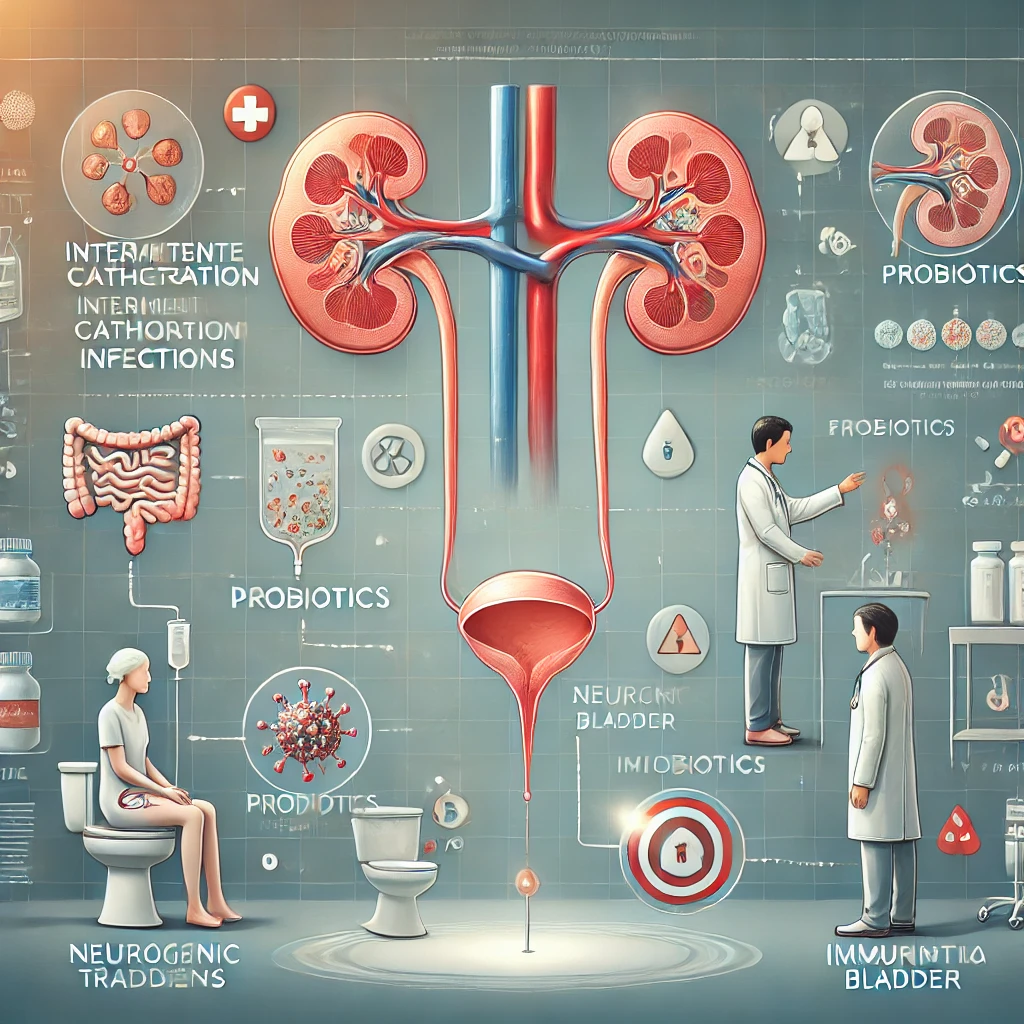
Effective bladder drainage is crucial to prevent UTIs and renal complications in NGB. Clean intermittent catheterization (CIC) is preferred when feasible, as it is associated with the lowest UTI rates. Alternatives include condom catheters (for low bladder pressures) and closed drainage systems (for intraurethral or suprapubic catheters). Catheters should be changed monthly to prevent biofilm formation.
2. Overnight Bladder Drainage:
Continuous overnight drainage via an intermittent catheter may reduce UTIs by decompressing the bladder. Limited studies show promise, especially in children, but more research is needed.
3. Bowel Management:
Optimizing bowel function, including addressing neurogenic bowel conditions, may reduce UTIs. Studies suggest significant decreases in UTI rates with improved bowel management.
4. Antibiotic Prophylaxis:
The use of antibiotics for UTI prevention is controversial due to risks of resistance. While continuous prophylaxis is not recommended for most, alternating antibiotics has shown efficacy in reducing infection rates in some populations.
5. Bladder Irrigation or Instillation:
Instillation of agents like gentamycin or povidone-iodine and repair of the bladder’s glycosaminoglycan (GAG) layer with hyaluronic acid and chondroitin sulfate have shown some benefits but require further research.
6. Cranberry and D-Mannose:
Cranberry and D-Mannose may prevent bacterial adherence in the bladder. Results are mixed- while some studies report benefits, others find no significant impact.
7. Probiotics:
Probiotic use has shown limited efficacy in UTI prevention for NGB. Intravesical administration may be promising, but more studies are needed.
8. Bacterial Interference:
Colonization with non-pathogenic E. coli reduces UTI rates, but therapies are not yet commercially available.
9. Immunotherapy:
Oral immunotherapy may prevent UTIs by enhancing immune responses, but more research is necessary to confirm efficacy.
10. Microbiome Research:
Emerging studies on the urinary microbiome (urobiome) suggest its role in UTI prevention and bladder health. Future therapies may focus on restoring a healthy urobiome through probiotics or other interventions.
11. Surgical Interventions:
Procedures like Botox injections, sacral neuromodulation, and augmentation cystoplasty may improve bladder function and reduce UTI risk, but recurrent infections remain an issue. Post-surgical bladder irrigation may help.
Future Directions:
Ongoing research focuses on novel therapies, such as urobiome-based treatments and advanced surgical techniques, to better manage and prevent UTIs in NGB patients.
Clinic Care Points for UTI in Neurogenic Bladder (NGB)
- Complications: UTIs in NGB can lead to serious outcomes like renal injury, urosepsis, or exacerbation of co-morbidities (e.g., autonomic dysreflexia). Prompt recognition and treatment of symptoms such as fever, back pain, new urinary incontinence, or pain with catheterization are crucial.
- Prevention Strategies: Baseline care involves proper catheter and bowel management. For recurrent UTIs, consider additional measures like bladder irrigation or probiotics.
- Ongoing Research: Techniques like immunotherapy are under study, so staying updated on current literature is essential for managing NGB patients effectively.
For further details-
Share this blog to social media:
Tags:
Suggested post
No post related to the current post. Please click on 'view more' to see more posts
